Tobacco Harm Index
Tobacco consumption remains one of the most persistent public health challenges in Europe, despite long-term declines in smoking prevalence. Across OECD member states, daily smoking among adults fell from an average of 21% in 2011 to 16% in 2021 (OECD, 2024). Yet tobacco use continues to impose substantial health and economic burdens: in OECD countries, smoking-related diseases accounted for an estimated 1.25 million deaths in 2022 (OECD, 2025). Beyond mortality, tobacco use contributes to chronic disease, hospitalisations, productivity losses, and broader societal costs.
In the Czech Republic, the economic burden of smoking has been quantified through cost-of-illness studies. Total costs from smoking in 2019 were estimated at approximately €2.1 billion (0.94% of GDP), with the largest share driven by indirect costs related to premature mortality (Landovská, 2025). While these figures are essential for understanding the scale of harm, such studies are complex, infrequently updated, and difficult to communicate beyond expert audiences. This creates a practical challenge for policymakers: the issue is not only the magnitude of tobacco-related harm, but also the lack of a simple, transparent, and regularly updateable tool that can track how consequences of smoking evolve over time and respond to policy changes.
This challenge reflects a broader dilemma in tobacco regulation. Governments are expected to protect public health by reducing exposure to harmful products and limiting chronic disease costs, while also respecting individual autonomy and the principles of market functioning. As a result, effective tobacco policy requires evidence-based and proportionate regulation — and, importantly, tools that can support continuous evaluation of outcomes over time.
The OECD’s Regulatory Policy Outlook stresses that regulation should be grounded in evidence, include assessments of social, economic and health impacts, and be supported by stakeholder engagement and feedback mechanisms (OECD, 2025). Composite indicators provide a practical response to this agenda: they offer a structured and repeatable method to synthesise complex, multidimensional evidence into an interpretable signal that can be updated regularly and used for policy learning. Well-known examples include the Human Development Index (UNDP, 2025), the OECD Better Life Index, and the Environmental Performance Index (Brock et al., 2024; OECD, 2025). In the field of addictive behaviours, the Somerset Intelligence Alcohol Harm Index provides a practical example of a similar monitoring tool used to track harm trends over time (Somerset Intelligence, 2025). Importantly, composite indicators are not direct measurements of reality — they are analytical tools designed to synthesise information, track trends, and enable transparency and comparison over time.
Building on this approach, the Tobacco Harm Index (THI) was developed as a composite monitoring tool for the Czech Republic. Rather than producing a monetary estimate of costs, the THI aggregates indicators across four domains — crime and shadow market activity, hospitalisations, mortality, and prevalence — into a single score that can be updated annually. The THI is therefore best understood as an indicative public policy tool: it complements cost-of-illness studies and other economic evaluations, while providing a clear way to monitor how tobacco-related harm changes over time and which domains drive these developments.
By offering a transparent and regularly updateable signal, the THI supports evidence-informed discussion about tobacco regulation and helps identify where policy attention may be most needed. The following sections summarise the methodology, key results, and interpretation of the index, and provide an overview of our next steps and ongoing work.
Methodology
The THI is designed as an annual monitoring tool that summarises the societal consequences of tobacco consumption in the Czech Republic using a transparent composite indicator approach. The index combines publicly available indicators across four domains into a single score that can be tracked over time and interpreted both by policymakers and the wider public. Importantly, THI does not estimate monetary costs or welfare losses; it provides an interpretable signal of trends in tobacco-related outcomes and their drivers.
Structure: four domains of tobacco-related consequences
THI is composed of four subindices reflecting distinct domains of tobacco-related consequences:
- Prevalence and exposure (weight 0.1). Captures behavioural and exposure patterns, including smoking prevalence (overall and among youth), smoking intensity, passive smoking exposure, and related indicators.
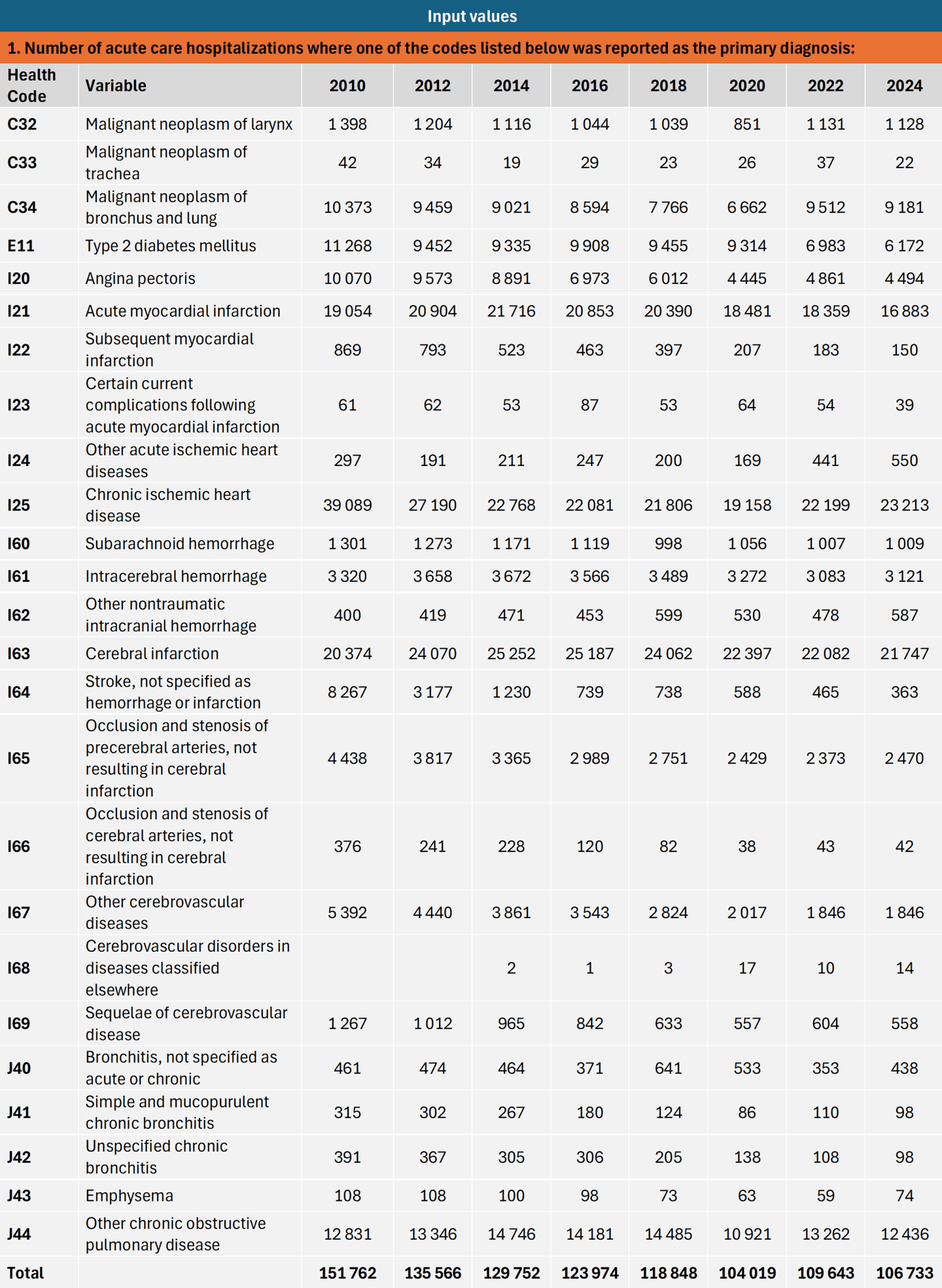
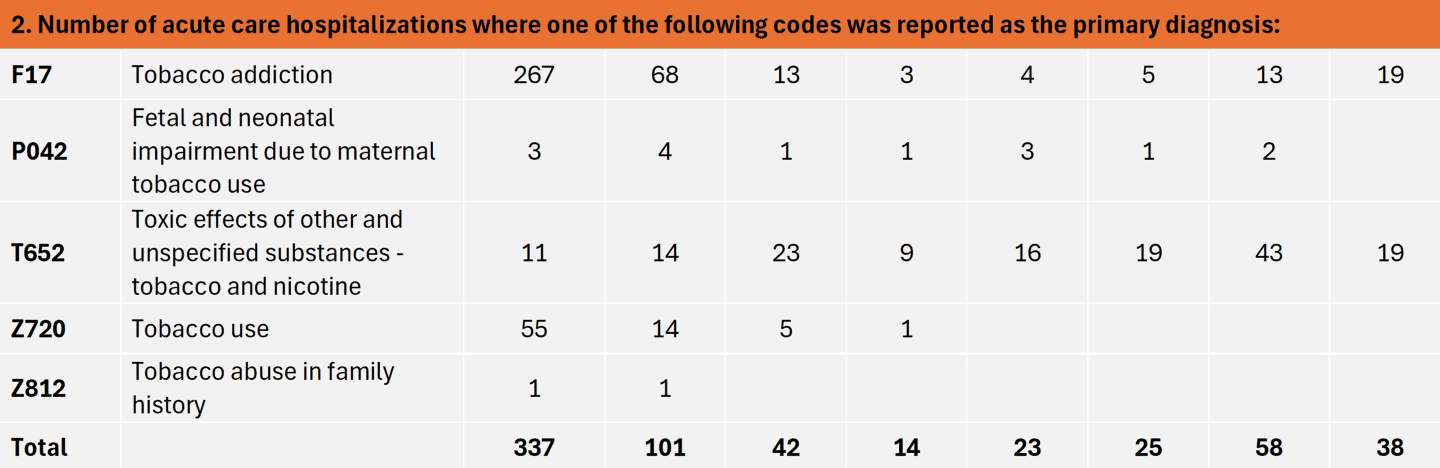
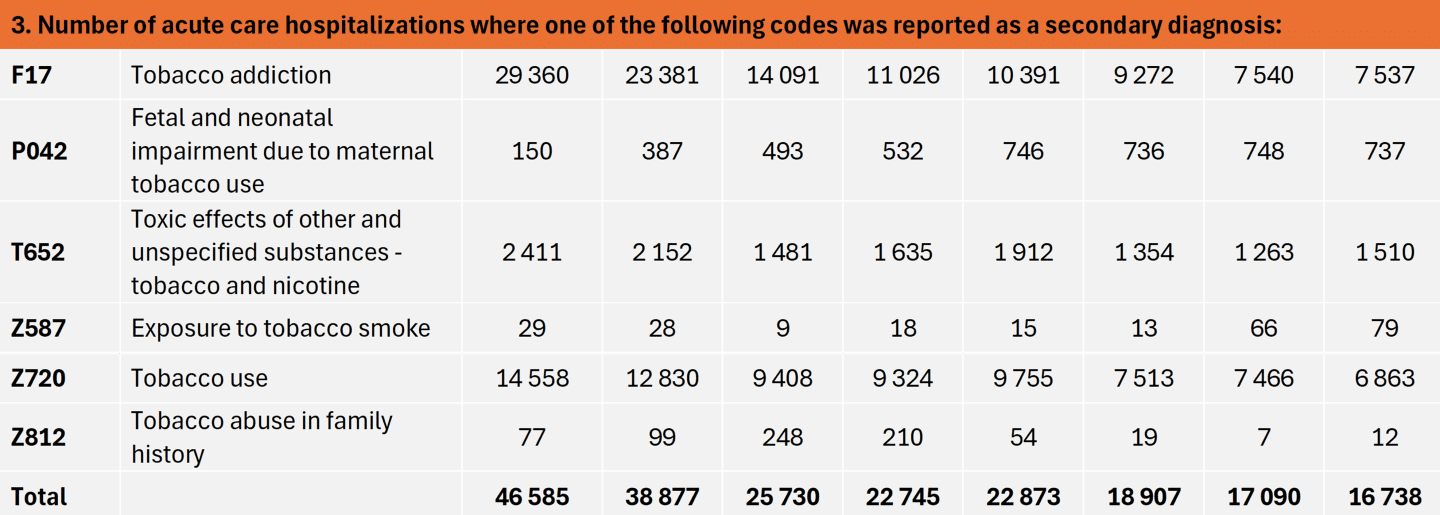
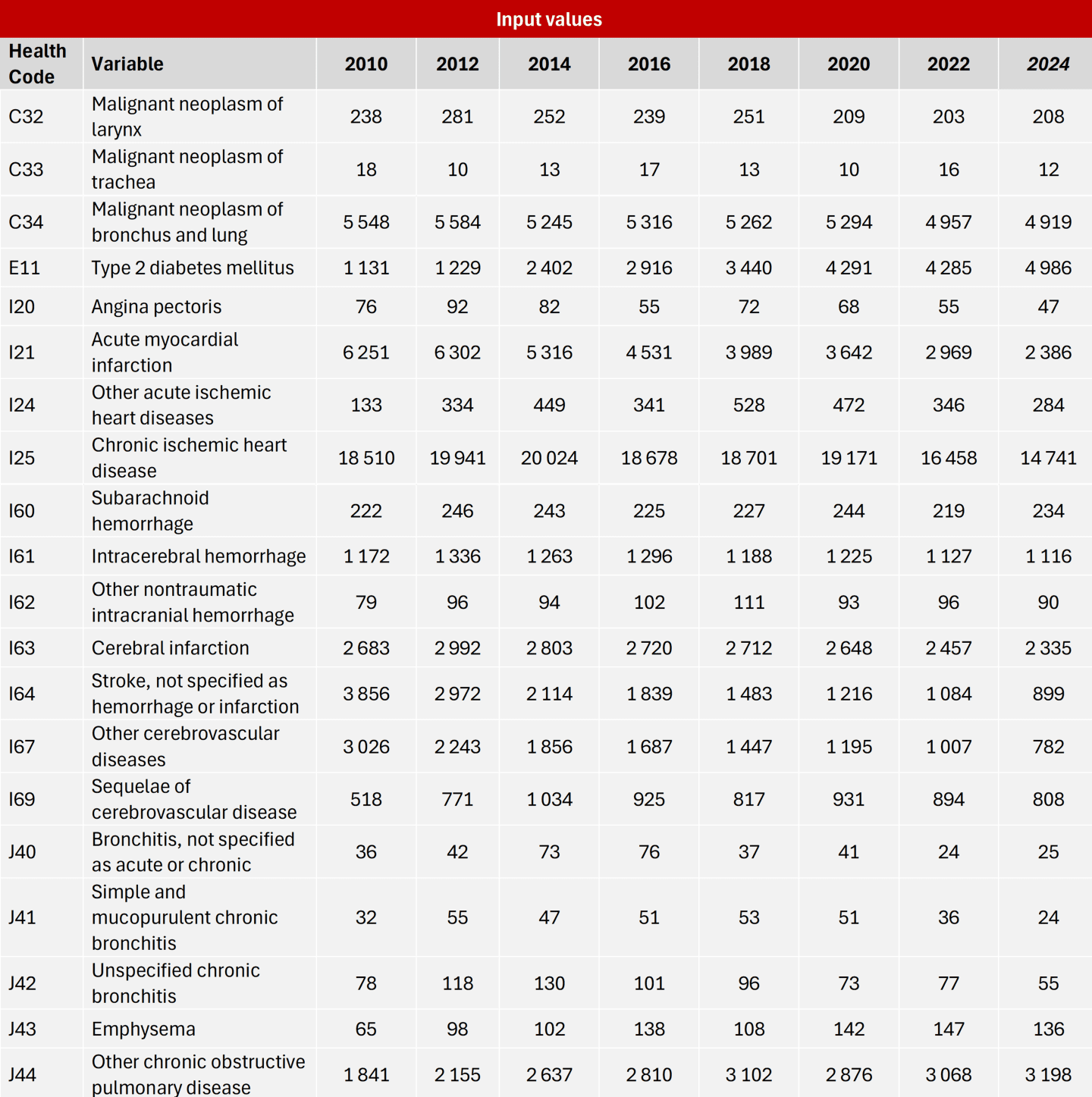
- Hospitalisations (weight 0.3). Tracks morbidity-related outcomes through hospitalisations associated with a set of diagnoses closely linked to smoking (including selected cancer, cardiovascular and respiratory diagnoses).
- Mortality (weight 0.5). Reflects the most severe outcomes — deaths associated with smoking-related causes.
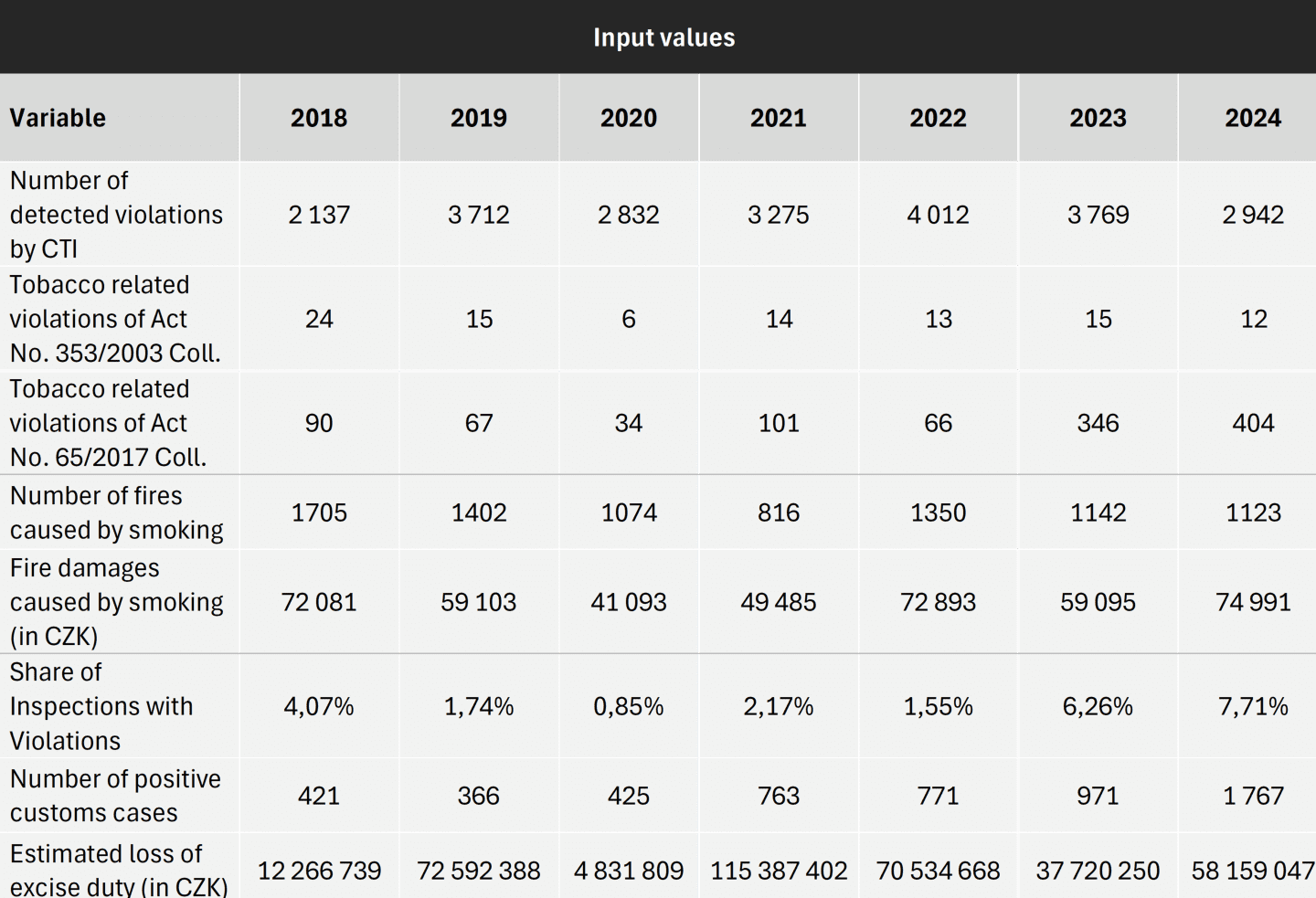
- Crime and shadow market (weight 0.1). Monitors enforcement and illicit market dynamics linked to tobacco, including violations of tobacco legislation, illicit trade and enforcement activity, estimated losses in excise duty, and smoking-related fires and fire-related damages.
Each subindex aggregates multiple indicators that are updated annually and drawn from official public sources.
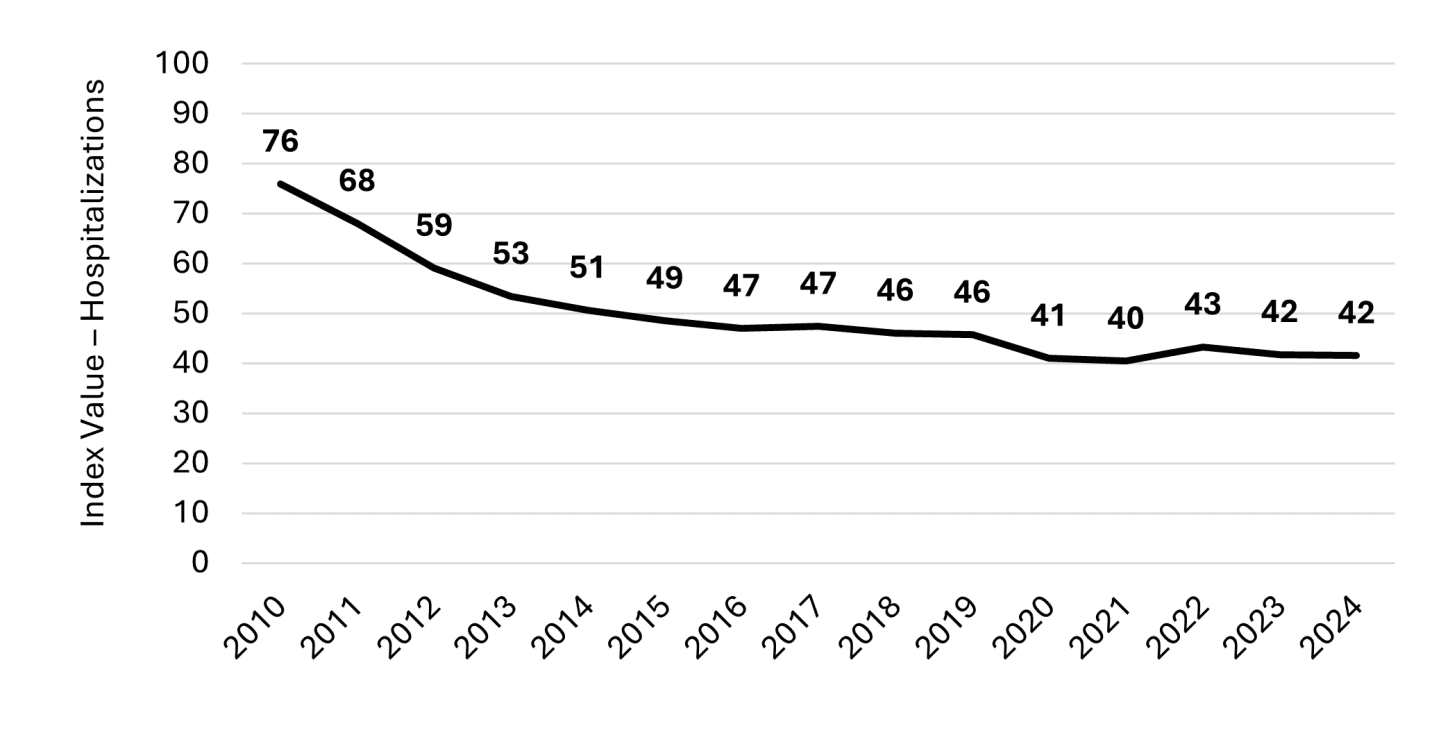
Data and indicator selection
Indicators were selected based on three core criteria:
- Policy relevance: indicators reflect outcomes that matter for public health and regulation.
- Data availability and consistency: indicators are available for multiple years and allow regular updates.
- Transparency: indicators come from official administrative or statistical sources and can be replicated.
The index is designed to be updateable on a yearly basis without relying on proprietary data or one-off research estimates.
Standardisation and aggregation
Because indicators are measured in different units (e.g., number of deaths, hospitalisations, prevalence rates), THI follows a standard composite index approach:
- Standardisation (z-scores): each indicator is transformed into a comparable scale using z-score standardisation to make different units comparable.
- Subindex construction: standardised indicators are averaged within each domain to create subindex scores. Within each subindex, indicators are treated with equal weight to preserve simplicity and transparency.
- Overall index construction: subindices are combined into the overall THI using explicit weights reflecting relative severity and policy relevance, with mortality receiving the highest weight.
- Rescaling for interpretation (T-scores): the final scores are rescaled to a 0–100 scale to support intuitive communication. In this format, higher values indicate more adverse tobacco-related outcomes relative to the baseline period, and the index can be tracked consistently over time.
Interpretation of scores
THI is primarily designed for trend monitoring:
- It shows whether overall tobacco-related consequences are increasing or decreasing relative to a baseline.
- It allows decomposition into domains to identify what drives change (e.g., whether trends are driven more by prevalence, morbidity, mortality, or illicit market dynamics).
- It supports structured policy discussion and evaluation, particularly when combined with other evidence such as cost-of-illness studies or programme evaluations.
Limitations
As a composite monitoring tool, THI has several limitations:
- It does not estimate outcomes in monetary terms and should not be interpreted as a cost measure.
- Results depend on indicator selection and weighting choices, which are made transparently but still involve judgement.
- The index captures observed trends and does not attribute causality to specific interventions without additional evaluation methods.
For these reasons, THI is best used alongside complementary tools such as cost-of-illness estimates, program evaluations, and qualitative policy analysis.
Results and Interpretation
This section presents the results of the (THI and interprets observed trends in the societal consequences of tobacco consumption in the Czech Republic. Results are shown graphically to support intuitive interpretation over time and are complemented by summary tables that document the underlying indicators and data sources used in each subindex. This dual presentation is intended to balance accessibility with transparency.
The results should be interpreted as trends in observed outcomes, not as causal estimates of the impact of specific policies. Changes in the index reflect how tobacco-related consequences evolve over time and may be influenced by multiple factors, including regulation, behaviour, market developments, and broader social and economic conditions.
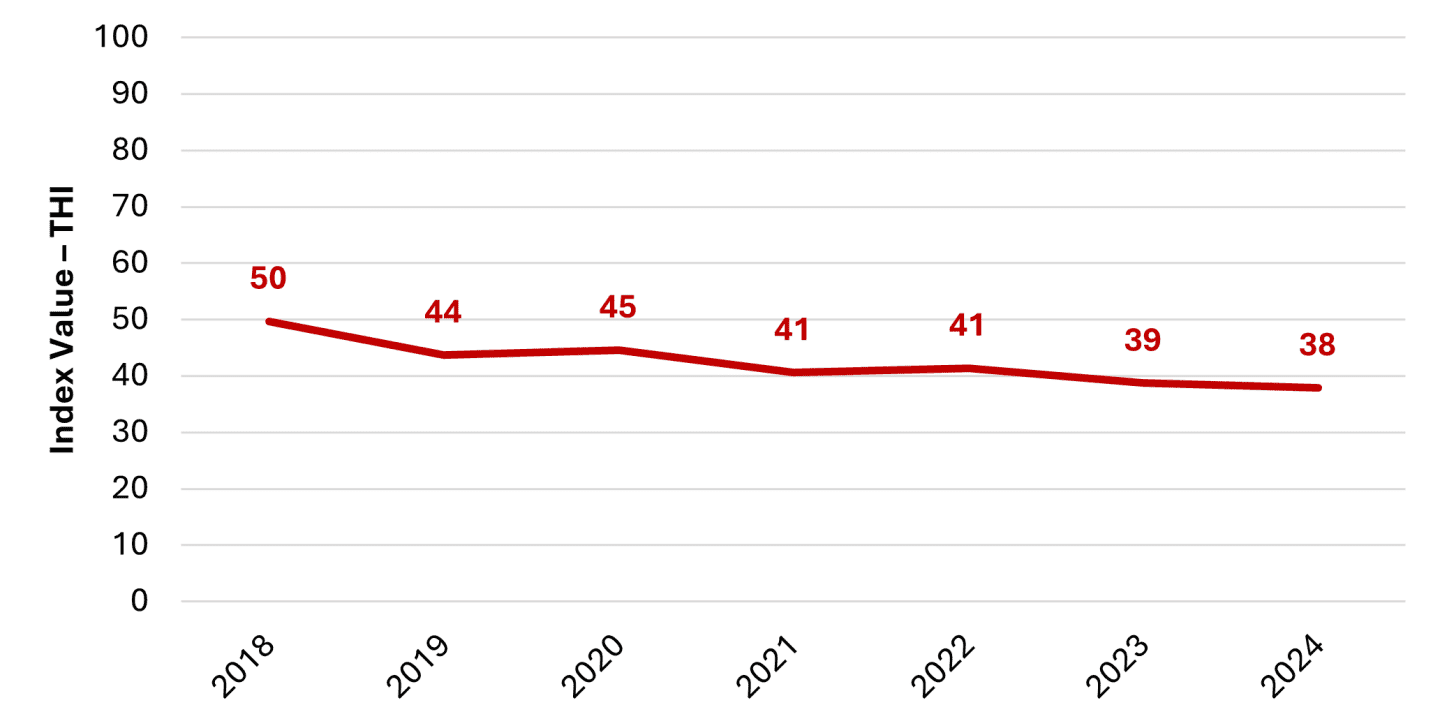
Overall Tobacco Harm Index (THI)
The overall Tobacco Harm Index shows a gradual decline in the societal consequences of tobacco consumption in the Czech Republic over the observed period. Following a more pronounced decrease between 2018 and 2019, the index remains relatively stable, with a slow downward trend continuing through to 2024.
This pattern suggests that, at an aggregate level, tobacco-related outcomes have been improving modestly over time rather than changing abruptly. The absence of sharp fluctuations indicates that developments in tobacco-related consequences are largely driven by structural and long-term factors, such as gradual changes in smoking behaviour, population health, and market dynamics, rather than short-term shocks.
At the same time, the relatively flat trajectory in recent years highlights that progress has been incremental rather than transformative. This underlines the importance of examining the individual subindices to understand which domains contribute most to the observed trend and where progress may be slowing or uneven across different dimensions of tobacco-related consequences.
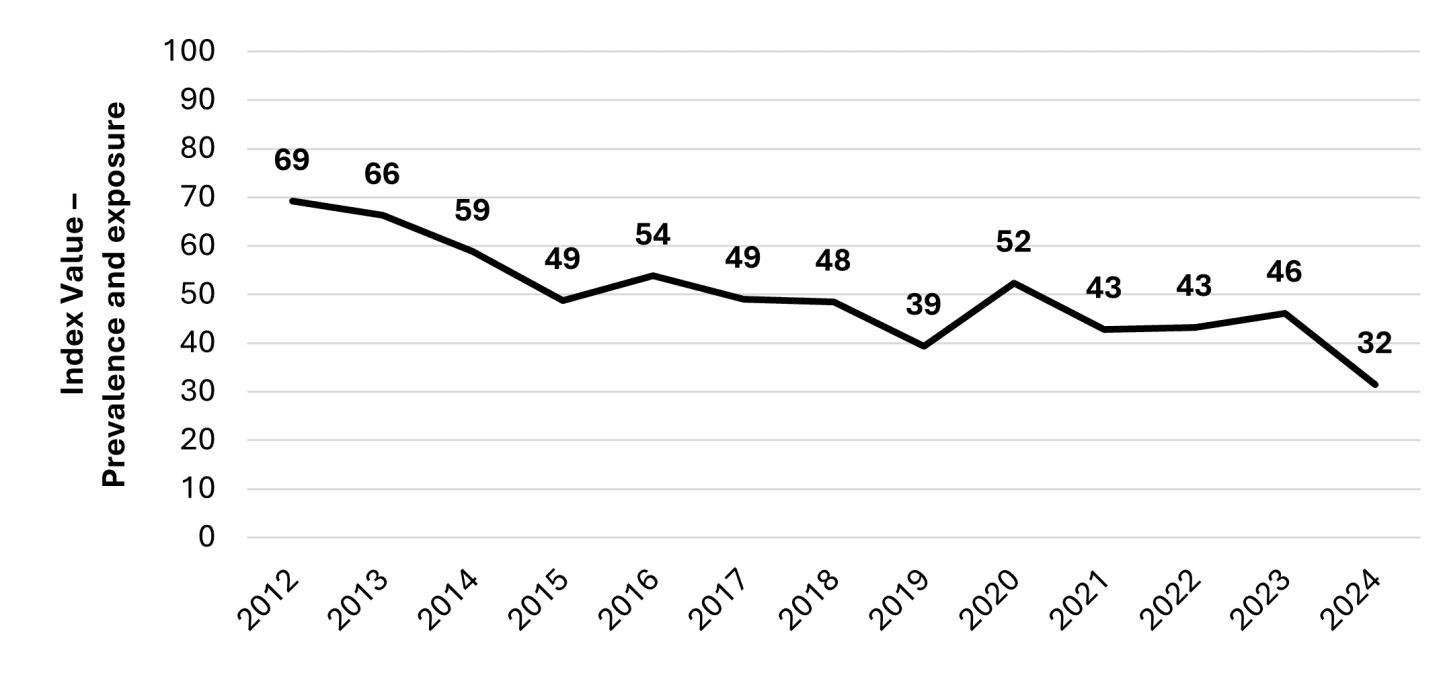
Subindex 1: Prevalence and Exposure
The prevalence and exposure subindex captures behavioural and exposure-related consequences of tobacco consumption, including smoking prevalence in the adult population and among young people, smoking intensity, and exposure to second-hand smoke. Unlike health outcomes, indicators in this domain tend to respond more quickly to changes in behaviour, social norms, economic conditions, and policy measures.
The trend shown in the graph indicates a gradual decline in prevalence and exposure-related outcomes over time, although with some variation across years. This pattern suggests a slow but persistent reduction in population-level exposure to tobacco, rather than abrupt shifts driven by short-term factors.
Because prevalence and exposure act as leading indicators, developments in this subindex provide important context for interpreting trends in hospitalisations and mortality. Sustained declines in prevalence and exposure today are likely to translate into improvements in morbidity and mortality only with a time lag, reflecting the cumulative nature of smoking-related disease.
At the same time, periods of stagnation or slower improvement in this subindex may signal risks for future health outcomes. For this reason, the prevalence and exposure domain plays a critical role in the Tobacco Harm Index by linking short- to medium-term behavioural developments with longer-term health-related consequences.
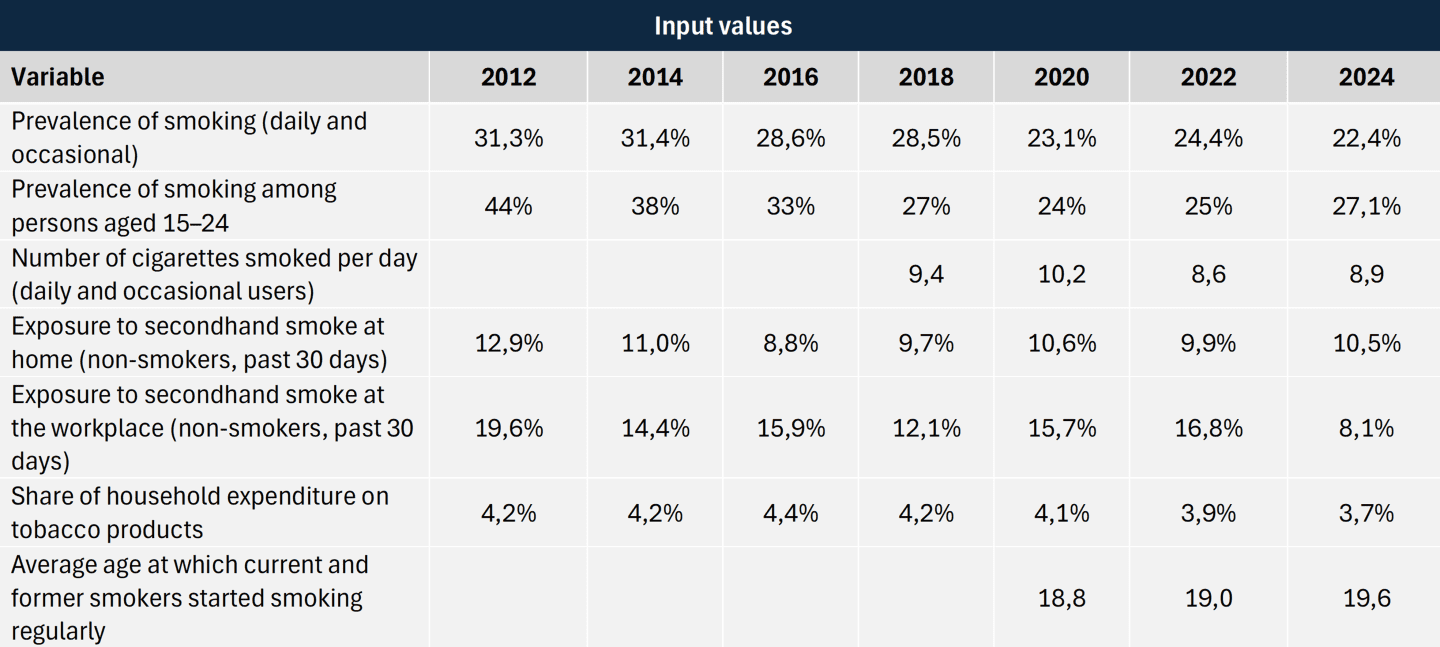
Subindex 2: Hospitalisations
The hospitalisations subindex reflects morbidity-related consequences of tobacco consumption, capturing trends in hospital admissions associated with diagnoses closely linked to smoking, including selected cardiovascular, respiratory, and oncological conditions.
The trend shown in the graph indicates a gradual decline in tobacco-related hospitalisations over time, without pronounced short-term fluctuations. This pattern is consistent with the long-term and cumulative nature of smoking-related morbidity, where changes in health outcomes typically follow changes in behaviour and exposure with a significant time lag.
Unlike prevalence-related indicators, hospitalisation trends tend to respond slowly to policy and behavioural change. As a result, short-term policy measures are unlikely to produce immediate visible effects in this subindex. Instead, sustained downward trends are more indicative of structural improvements in population health, potentially reflecting long-term reductions in smoking prevalence, changes in smoking intensity, or improvements in prevention and cessation.
At the same time, the relatively smooth trajectory of this subindex highlights the importance of interpreting hospitalisation data in conjunction with other domains. While declining morbidity-related outcomes are encouraging, they need to be assessed alongside developments in prevalence and mortality to obtain a comprehensive picture of tobacco-related consequences.
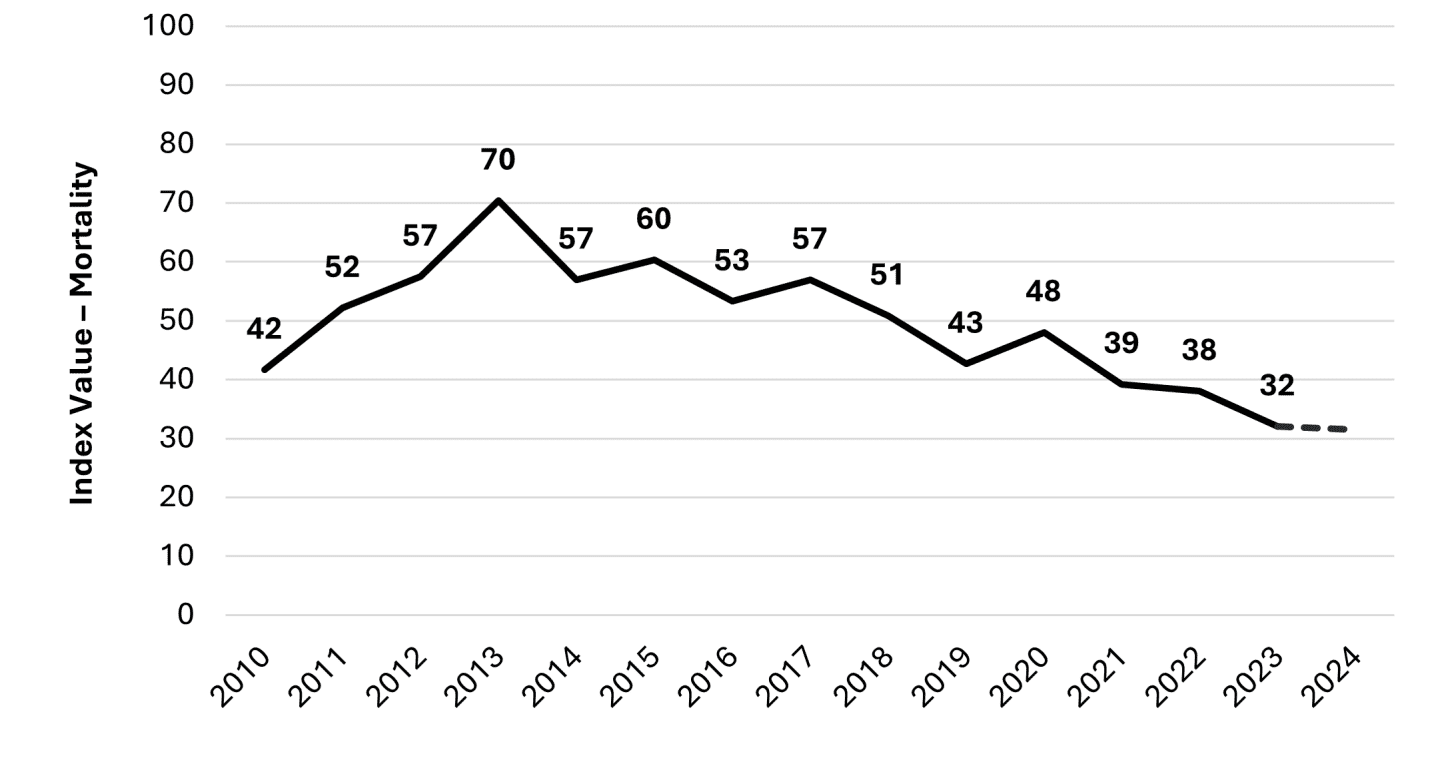
Subindex 3: Mortality
The mortality subindex captures the most severe and irreversible consequences of tobacco consumption — deaths associated with smoking-related causes. Given the societal significance of this outcome, mortality carries the highest weight within the overall Tobacco Harm Index.
The trend in the graph shows a two-phase pattern: mortality-related outcomes increase up to around 2013, followed by a gradual decline in the subsequent years. This trajectory is consistent with the long-term and cumulative nature of smoking-related mortality, where observed trends are shaped by historical exposure, demographic structure, and cohort effects rather than short-term developments.
As with hospitalisations, mortality outcomes typically respond to changes in smoking behaviour with a substantial time lag. The post-2013 decline may therefore reflect longer-run improvements in population exposure and risk factors, while the earlier increase highlights that adverse outcomes can continue to rise even as policy attention intensifies — underscoring the importance of continuous monitoring.
Overall, the mortality subindex provides essential context for interpreting developments in the other domains: it reflects slow-moving structural changes and helps anchor the overall THI in the most consequential tobacco-related outcomes.
Subindex 4: Crime and Shadow Market
The crime and shadow market subindex captures non-health-related consequences of tobacco consumption, focusing on enforcement activity, illicit trade, and related externalities. Unlike health outcomes, developments in this domain are closely linked to regulatory design, tax policy, enforcement intensity, and market incentives.
The trend shown in the graph suggests that developments in this area have been less uniform and more volatile than health-related outcomes. Periods of decline are interspersed with phases of relative stagnation or temporary increases, indicating that illicit market activity and enforcement outcomes respond differently to policy and economic conditions than smoking prevalence or health indicators.
Importantly, changes in this subindex should not be interpreted as a direct proxy for consumption levels. Increases may reflect stronger enforcement, shifts in smuggling routes, or changes in reporting practices, while decreases may indicate improved compliance or altered market incentives. As such, this subindex provides essential contextual information for interpreting the overall index and highlights the importance of considering unintended consequences when evaluating tobacco regulation.

Conclusion and Next Steps
The Tobacco Harm Index provides a structured overview of how the societal consequences of tobacco consumption in the Czech Republic have evolved over time. By combining information on prevalence and exposure, morbidity, mortality, and crime and shadow market dynamics, the index highlights that improvements in tobacco-related outcomes have been gradual and uneven across domains, rather than abrupt or uniform.
The results suggest that while population-level exposure and selected health outcomes have shown a slow downward trend in recent years, progress has been incremental rather than transformative. At the same time, developments in non-health domains — particularly crime, enforcement, and illicit market activity — illustrate that regulatory outcomes extend beyond health indicators alone and may reflect unintended consequences, enforcement intensity, or market responses. Taken together, these findings underline the value of a multi-dimensional monitoring approach when evaluating tobacco policy.
Importantly, the THI is not designed to estimate monetary costs or welfare losses, nor to attribute causal effects to individual policy measures. Instead, it serves as an indicative monitoring tool that complements cost-of-illness studies, programme evaluations, and other forms of economic and policy analysis. Its primary contribution lies in enabling transparent, regular, and interpretable tracking of tobacco-related outcomes over time, in line with evidence-based policymaking and better regulation principles.
Next steps
The THI is conceived as a living framework rather than a one-off exercise. Key next steps include:
- Regular annual updates of the index as new data become available, enabling continuous monitoring of trends in tobacco-related outcomes.
- Further refinement of indicators and data sources, particularly in areas where reporting practices, definitions, or data coverage evolve over time.
- Refinement of weighting schemes, both at the level of subindices and at the level of individual indicators within each domain. This process will be informed by structured input from subject-matter experts in public health, health economics, epidemiology, enforcement, and regulatory policy, with the aim of strengthening conceptual validity while maintaining transparency.
- Sensitivity and robustness analysis to assess how alternative weighting assumptions and methodological choices influence results and interpretation.
- Exploration of comparative extensions, including the potential application of the framework to other countries or to related policy domains.
In parallel, ongoing work focuses on embedding the THI more closely into broader discussions on tobacco and nicotine policy, regulatory evaluation, and public communication.
Full working paper available ZDE.
Sources
- Block, S., Emerson, J. W., Esty, D. C., de Sherbinin, A., Wendling, Z. A., et al. (2024).
Environmental Performance Index 2024. Yale Center for Environmental Law & Policy. - Landovská, P. (2025). Social costs of smoking in the Czech Republic. Applied Health Economics and Health Policy, 23(1), 141–153.
- OECD (2024). Society at a Glance 2024: OECD Social Indicators. OECD Publishing, Paris.
- OECD (2025). Better Life Index / Well-being Data Monitor.
- OECD (2025). Health at a Glance 2025: OECD Indicators. OECD Publishing, Paris.
- OECD (2025). OECD Regulatory Policy Outlook 2025. OECD Publishing, Paris.
- Somerset Intelligence (2025). Alcohol Harm Index.
- United Nations Development Programme (2025). Human Development Index (HDI). Human Development Reports.